Postpartum care kicks off right after delivery and stretches through the first six weeks, a time when your body rebuilds from the marathon of pregnancy and birth. In India, traditional practices blend with modern guidelines to support new mothers through physical aches, hormonal shifts, and baby bonding. Every new mom deserves focused attention to sidestep complications like infections or mood dips. Physical Recovery Basics The uterus contracts back to pre-pregnancy size over six weeks, causing afterpains that feel like cramps, especially during breastfeeding. Vaginal lochia discharge starts heavy and red, lightening to spotting by week four—use pads, not tampons, to avoid infections. C-section moms face incision care: keep dry, watch for redness or pus, and ease into walking to prevent clots. Perineal soreness from tears or episiotomy heals with cold packs first 48 hours, then warm sitz baths. Constipation hits hard from pain meds and iron supplements; stool softeners and fiber help without straining. Breast engorgement peaks day 3—frequent nursing or pumping relieves it. Pelvic floor exercises like Kegels start gently week 2 to rebuild strength. In humid Indian climates, hygiene trumps all: daily showers, loose cotton clothes reduce thrush risks. National guidelines recommend check-ups day 3, 7, and 6 weeks for vitals, hemoglobin. Nutrition for Healing New moms burn 500 extra calories daily if breastfeeding, so nutrient-dense meals fuel recovery. Iron-rich greens like spinach, lentils (dal), and jaggery combat anemia common post-blood loss. Protein from eggs, paneer, fish rebuilds tissues; calcium via ragi, milk prevents bone loss. Hydrate 3-4 liters daily for milk supply and constipation relief. Traditional postpartum diets emphasize warm, ghee-laden foods: moong dal khichdi, oats porridge soothe digestion. Avoid gas-causing raw salads initially. Omega-3s from walnuts, flaxseeds ease inflammation. Supplements: continue folic acid, add vitamin D for urban moms low on sun. Small, frequent meals curb fatigue. Ayurvedic touches like turmeric milk boost immunity, but balance with variety to hit 2,500 calories. Track weight loss: 0.5kg/week safe post-week 2. Consult a gynecologist for personalized plans. Emotional Wellness Baby blues strike 80% with tears, anxiety days 3-10 from hormone drops—family support normalizes it. Postpartum depression affects 15-20% Indian moms, longer sadness, withdrawal signaling need for help. Sleep deprivation amplifies; nap when baby naps. Journaling or walks release endorphins. Joint family systems aid, but modern isolation worsens. Talk openly; husbands share chores. Yoga pranayama calms week 4 onward. Severe signs like harmful thoughts demand immediate care. Exercise and Activity Rest rules first two weeks: no lifting over baby weight. Week 3, short walks prevent clots. Post-6 weeks, postnatal yoga rebuilds core—bridge pose for pelvic floor. Swimming suits humid weather but post-clearance. Aim 150 minutes moderate activity weekly by month 3. Kegels: contract 10 seconds, 10 reps thrice daily. Avoid crunches till 8 weeks. Listen to body; pain means stop. Consult gynecologist before starting. Breastfeeding Essentials Latch correctly to avoid sore nipples: baby’s mouth wide, chin tucked. Colostrum first 3 days nourishes immunity. Cluster feeds normal growth spurts. Pumps help if returning work. Store milk fridge 4 days. Supplements like fenugreek boost supply culturally, but hydrate first. Mastitis signs: fever, red streaks—warm compress, continue nursing. Month 1 exclusive best for baby gut health. Common Complications Watch heavy bleeding (>1 pad/hour), foul lochia, fever>100.4F—infection flags. Preeclampsia lingers as headaches, swelling. DVT leg pain risks post-C-section. Mastitis, thyroid issues common. UTI from catheters. Early reporting saves lives. In India, anemia delays recovery; check hemoglobin. High-risk like diabetics need closer watch. Family Planning and Check-ups Discuss contraception at first visit: condoms, pills safe post-6 weeks. IUDs post-check. Space pregnancies 2-3 years optimal. 6-week exam clears exercise, sex. Home-based newborn care visits screen both. Track baby weight, jaundice. (Word count: 1,823) FAQ How long does postpartum bleeding last? 4-6 weeks, lightening gradually. When to resume exercise? Gentle walks week 2, full after 6-week check. What causes baby blues? Hormone shifts; resolves in 2 weeks.
Menopause and Sexual Health – How to Maintain Intimacy After 40
Menopause: a natural shift, not the end of intimacy Menopause marks the end of menstrual cycles, but it is so much more – a time when hormone levels, especially estrogen, drop significantly, affecting every part of a woman’s body, including sexual health. For many Indian women after 40, this brings changes like vaginal dryness, discomfort during intercourse, reduced desire and sometimes painful sex. These are not just “normal aging”; they are direct results of hormonal shifts, and the good news is they can often be managed to restore comfort and pleasure. In India, where cultural taboos around discussing sex persist, many women suffer silently, assuming intimacy is over. But studies show menopause impacts sexual function across domains like interest, lubrication and orgasm, yet with open conversation and practical steps, intimacy can not only be maintained but enriched. The hormonal changes behind sexual challenges As perimenopause begins (often in the 40s), estrogen and progesterone fluctuate wildly, then decline sharply at menopause. Estrogen is key for vaginal health – it keeps tissues plump, elastic and lubricated. Without it: Vaginal walls thin (atrophy), becoming dry and fragile. Natural lubrication decreases, making arousal slower or painful. Blood flow to the genitals reduces, affecting sensation and orgasm. Testosterone, important for desire, also dips, compounded by stress, sleep issues and body image changes. Indian research notes perimenopausal women often have better function than postmenopausal, with lubrication and orgasm hit hardest post‑menopause. Common sexual symptoms after 40 Vaginal dryness and discomfort (dyspareunia): Up to 55% of postmenopausal women report pain due to lack of moisture. Low desire (libido): 40–55% experience reduced interest, linked to hormones, fatigue and relationship dynamics. Delayed arousal and orgasm: Slower response, less intense climaxes from tissue changes. Bladder issues: Frequent UTIs or urgency, further deterring intimacy. These symptoms compound if unaddressed, leading to avoidance and relationship strain. But they are treatable. Emotional and relational aspects Intimacy is 20% physical, 80% emotional. After 40, body changes can dent confidence, while life stresses (children, career, caregiving) sap energy. Partners may not understand, assuming disinterest means rejection. Indian women often face added layers – family expectations, lack of privacy, cultural silence on menopause sex. Yet, studies show partner satisfaction remains stable if communication opens up and consult a Gynecologist. Practical steps to restore lubrication and comfort Moisturisers and lubricants Vaginal moisturisers (used daily) hydrate tissues; lubricants (during sex) reduce friction. Water‑based or silicone‑based work well. Pelvic floor exercises (Kegels) Strengthen muscles for better blood flow and sensation. Do 10–15 reps daily. Hormonal options Local estrogen creams/rings restore vaginal health without systemic risks. Lifestyle tweaks Stay hydrated, limit alcohol/caffeine. Yoga/meditation reduces stress, boosts desire. Reigniting desire and pleasure Extended foreplay: Focus on kissing, touching; arousal takes longer. New positions: Avoid deep penetration if painful. Solo exploration: Vibrators/masturbation rebuilds connection to body. Couples therapy: Address communication gaps. FAQ Can sexual desire return naturally after menopause? Yes, for many, desire fluctuates but can stabilise with hormone balance, stress reduction and open partner talk. Therapy and lifestyle changes help 80% see improvement. Is hormone therapy safe for sex after 40? Local options like creams are low‑risk and effective for dryness. Discuss systemic HRT with your doctor. How do Indian women handle menopause intimacy taboos? Start private conversations with trusted friends/partners; seek gynaecologist advice. Education empowers.
Yeast Infections vs. Bacterial Vaginosis – How to Tell the Difference
Vaginal itching, discharge, and discomfort are very common reasons women visit a gynaecologist in India. Most of the time, the culprit is either a yeast infection (vulvovaginal candidiasis) or bacterial vaginosis (BV)—two different conditions that feel similar but need completely different treatments. Taking the wrong over‑the‑counter medicine can actually make symptoms worse or keep the problem recurring. Understanding the differences in discharge, odour, associated symptoms, and triggers helps women know when to suspect yeast vs BV and why a proper medical diagnosis matters. What Is a Yeast Infection? A vaginal yeast infection happens when Candida, a fungus that normally lives in small amounts in the vagina, overgrows and irritates the tissues. Typical features: Thick, white, curd‑like (“cottage cheese”) discharge. Intense itching, burning, redness, and swelling of the vulva. Burning during urination or sex due to irritated skin. Yeast infections are not sexually transmitted infections in the traditional sense; they are often linked to antibiotics, tight clothing, high sugar levels, hormonal changes, or moisture. What Is Bacterial Vaginosis (BV)? BV happens when the balance of vaginal bacteria is disturbed and “good” lactobacilli decrease, allowing overgrowth of other bacteria. Key features: Thin, gray, white, or sometimes yellow/greenish discharge that can be more noticeable after sex. A strong fishy odour, often worse after intercourse or during periods. Mild itching or burning; many women have no symptoms at all. BV is not classified as a classic STI, but sexual activity, new partners, or multiple partners increase risk because they alter the vaginal environment. Symptom Comparison: Yeast vs BV Although both cause “vaginitis” (vaginal inflammation), their signature signs differ. Discharge BV: Usually thin, watery, gray or white, sometimes yellowish/greenish; tends to coat the vaginal walls and may be more evident after sex. Yeast: Typically thick, white, clumpy discharge, often described as looking like cottage cheese; usually with very little odour. Odour BV: Distinctive “fishy” smell, which may intensify after intercourse or during menses. Yeast: Usually no strong odour; if present, it is not typically fishy. Itching, Redness, and Pain BV: Itching may be mild or absent; vulval redness is often minimal. Yeast: Intense itching, redness, swelling, soreness of the vulva are very common, with burning on urination or sex. pH (for clinicians) BV: Vaginal pH usually >4.5. Yeast: Vaginal pH usually normal (≤4.5). Common Triggers and Risk Factors Yeast Infection Triggers Recent antibiotic use, which kills protective bacteria and allows Candida to overgrow. High blood sugar in diabetes or frequent sugary foods. Tight, synthetic underwear, damp clothing, and excessive heat and humidity. Hormonal factors: pregnancy, oral contraceptives, high‑oestrogen states. BV Risk Factors New sexual partner or multiple partners, lack of condom use. Vaginal douching or use of harsh washes that disrupt natural flora. Smoking, and sometimes intrauterine devices (IUDs) in some studies. Both conditions are more likely when the natural vaginal balance is disturbed, but the organisms and treatments differ, so accurate diagnosis is important. Why Self‑Diagnosis Can Be Tricky Many women assume that any itching equals a yeast infection and buy antifungal creams without testing. However, symptom overlap means this can easily go wrong: BV and yeast can both cause discharge and some itching. Up to half of BV cases can be asymptomatic, discovered only on testing. Mixed infections (BV + yeast) also occur, especially in high‑risk or recurrent cases. Repeated wrong treatment may worsen irritation, alter pH further, and allow resistant organisms to thrive. Persistent or recurrent symptoms always deserve professional evaluation. How Doctors Differentiate Yeast Infection and BV In clinic, your provider may: Take a detailed history – onset, type of discharge, odour, triggers, hygiene practices, sexual history, recent antibiotics. Perform a pelvic examination – assess colour, consistency, and smell of discharge; inspect vulval skin for redness, cracks, or sores. Check vaginal pH – elevated in BV, usually normal in yeast infection. Examine a sample under the microscope – clue cells and lack of lactobacilli in BV, budding yeast and pseudohyphae in candidiasis. Use swabs, culture, or molecular tests in recurrent or unclear cases. Accurate diagnosis guides the right treatment and helps break the cycle of recurrence. Treatment Differences: Why It Matters Because causes differ, treatments do too. Treating Yeast Infections Antifungal medications – topical azole creams, pessaries, or oral tablets, usually for a few days. For recurrent infections, longer courses or maintenance regimens may be needed. Supportive steps: Keep vulval area dry; avoid perfumed products and tight clothing. Manage blood sugar if diabetic. Treating Bacterial Vaginosis Antibiotics (oral or vaginal), usually metronidazole or clindamycin in various regimens. Some women experience recurrences; extended or intermittent regimens may be advised. Supportive steps: Avoid douching and harsh cleansers; use mild, unscented products externally only. Discuss condom use and sexual practices that might repeatedly disturb flora. Using antifungals for BV will not fix the problem, and using BV antibiotics for yeast will not relieve the itch—hence the need to tell them apart. When to See a Doctor Seek medical care if: It is your first episode of unusual discharge or itching. You have fever, pelvic pain, or bleeding, which could indicate more serious infection. Symptoms keep coming back despite over‑the‑counter treatments. You are pregnant, diabetic, or immunocompromised. There is strong odour, greenish discharge, or pain in the lower abdomen. In India’s climate and close‑living conditions, recurrent vaginitis is common; long‑term relief requires a mix of correct diagnosis, tailored treatment, and lifestyle changes. FAQs 1) Can I have both a yeast infection and bacterial vaginosis at the same time? Yes. Mixed infections can occur, especially in women with frequent antibiotic use, uncontrolled diabetes, or repeated douching. In such cases, symptoms may be confusing—for example, thick discharge plus odour—and simple home treatment often fails. A clinician can confirm the combination with microscopy or lab tests and prescribe a plan that covers both organisms appropriately. 2) Will BV or yeast infection affect my fertility or pregnancy? Untreated BV has been associated with an increased risk of pregnancy complications, preterm birth, and post‑surgical infections after gynaecological procedures. Yeast infections mainly cause
Sexually Transmitted Infections (STIs) in Women – Testing and Prevention
Sexually transmitted infections (STIs) are not just a “youth issue” or something that happens to “other people.” In India, community‑based estimates suggest that more than 6% of adults experience an STI or reproductive tract infection each year, translating into tens of millions of episodes. Women carry a disproportionate share of the health impact: untreated STIs can lead to pelvic inflammatory disease, infertility, ectopic pregnancy, pregnancy complications, chronic pelvic pain, and an increased risk of HIV. The good news is that most STIs are preventable and many are easily treatable if diagnosed in time. This blog focuses on testing and prevention strategies for women, using concepts relevant to India’s public‑health approach. Common STIs Affecting Women STIs can be bacterial, viral, or parasitic. Important ones for women’s health include: Bacterial Chlamydia Gonorrhoea Syphilis Chancroid and other less common bacterial STIs Viral Human papillomavirus (HPV) Herpes simplex virus (HSV) Human immunodeficiency virus (HIV) Hepatitis B Parasitic / others Trichomoniasis Some vaginal infections that overlap with reproductive tract infections Many of these may not cause obvious symptoms, especially in women, which is why proactive testing is crucial. Why STIs Are a Major Concern for Women in India STIs increase the biological risk of acquiring and transmitting HIV; effective STI control is a recognised HIV‑prevention strategy. Estimates indicate that at any given time, around 40% of women may have some form of RTI/STI, but only about 1% complete full treatment along with their partners. Social stigma and lack of privacy mean women often delay care, self‑medicate, or seek help only when complications develop. Improving awareness of testing and prevention is essential to break this cycle. Typical Symptoms of STIs in Women (and Why Many Are Silent) Possible symptoms include: Unusual vaginal discharge (change in colour, smell, or quantity). Burning or pain during urination. Lower abdominal or pelvic pain. Itching, redness, or sores on the genital area. Pain or bleeding during or after sex. Irregular vaginal bleeding, including after intercourse. However: Many infections like chlamydia and early HIV can be asymptomatic or have very mild symptoms. Syndromic approaches (treating based on symptoms like discharge) may miss cervical infections in women. Therefore, regular screening in at‑risk women, not just symptom‑based treatment, is key. How Are STIs Diagnosed in Women? 1) Syndromic Management (Current Public‑Health Backbone in India) In many primary health centres and Suraksha/STI clinics, doctors use syndromic algorithms: they look at the pattern of symptoms (e.g., vaginal discharge, genital ulcer) and treat for the most likely infections without waiting for lab tests. This approach is cost‑effective and allows immediate treatment, which is vital where labs are limited. However, it can lead to both under‑diagnosis & over‑treatment, especially for cervical infections like chlamydia and gonorrhoea. 2) Etiological / Test‑Based Diagnosis (Growing Emphasis) Where lab facilities are available, more specific tests are used: Nucleic acid amplification tests (NAATs) for chlamydia and gonorrhoea. Blood tests for syphilis, HIV, and hepatitis B. Microscopy, culture, and point‑of‑care tests for trichomonas and others. National guidelines are gradually encouraging greater use of diagnostic testing and sentinel surveillance, especially as point‑of‑care tests become more affordable. Who Should Get Tested and When? Adapted from international recommendations and national strategies: Sexually active women under 25 – screen periodically for chlamydia and gonorrhoea, especially with new or multiple partners. Women over 25 with risk factors (new partner, multiple partners, partner with an STI, inconsistent condom use). Pregnant women – routine testing for syphilis, HIV, and often hepatitis B, sometimes chlamydia/gonorrhoea where feasible. Women with symptoms: discharge, ulcers, pelvic pain, or contact with someone known to have an STI. Women planning pregnancy or undergoing infertility evaluation. In India, STI/RTI clinics, antenatal clinics, and some gynaecology services integrate screening into routine reproductive health visits. Prevention Strategies: What Really Works 1) Safer Sexual Practices Correct and consistent condom use significantly reduces the risk of most STIs, including HIV. Mutual monogamy between partners who are both tested and uninfected. Avoiding high‑risk behaviours (multiple partners, unprotected sex with partners whose status is unknown). 2) Vaccination HPV vaccination helps prevent infections with high‑risk HPV types that cause cervical cancer and some genital warts. Hepatitis B vaccination reduces sexually and blood‑borne transmission and protects liver health. Vaccines do not replace condoms or testing but significantly lower specific infection risks. 3) Regular Screening and Early Treatment Proactive testing in sexually active women, even when asymptomatic, allows early cure for bacterial STIs and reduces onward transmission. Partner notification and treatment (including expedited partner therapy models discussed in emerging guidelines) can reduce re‑infection rates. 4) Education, Counselling, and De‑Stigmatisation Counselling about symptoms, risks, condom negotiation, and partner communication is an integral part of STI/RTI services under India’s National AIDS Control Programme. Reducing shame and fear encourages women to seek care earlier and complete treatment. Complications of Untreated STIs in Women If not diagnosed and treated promptly, STIs can cause: Pelvic inflammatory disease (PID) – infection spreading to uterus, tubes, ovaries. Infertility due to tubal damage or blockage. Ectopic pregnancy with life‑threatening bleeding. Chronic pelvic pain and painful intercourse. Pregnancy complications – miscarriage, stillbirth, premature labour, neonatal infections. Increased risk of HIV acquisition and transmission. These outcomes are largely preventable with robust testing and treatment coverage. STI Services and Public‑Health Approach in India (Snapshot) Under the National AIDS Control Programme, India has established a network of STI/RTI clinics (e.g., Suraksha Clinics) providing standardised syndromic management, counselling, partner management, and syphilis testing. Data suggest over 6% adult prevalence of STI/RTI episodes annually, but routine data are incomplete, and many women have infections without seeking formal care. National technical guidelines emphasise: Integrating STI care into reproductive and adolescent health services. Improving lab infrastructure and point‑of‑care testing. Sentinel surveillance to better understand trends and refine strategies. Practical Tips for Women Do not ignore persistent discharge, itching, pain, or bleeding—consult a qualified provider. Ask for confidential counselling and testing; government clinics often offer services free or at low cost. Ensure your partner is treated if advised; otherwise re‑infection is common. Keep a record of
What Does a Gynecologist Do? A Complete Guide to Women’s Reproductive Health
For many women, visiting a gynecologist in Pune might be a source of anxiety or confusion. However, gynecologists in Pune are essential partners in women’s health, guiding them through every stage of life from puberty through menopause. This comprehensive guide will explain who gynecologists are, what they do, and why regular visits are important for maintaining reproductive and overall health. Who is a Gynecologist? A medical doctor specialized in women’s reproductive system health. Trained to manage menstrual health, sexual health, fertility, pregnancy, childbirth, and menopause. Often also trained as obstetricians (OB-GYNs), handling pregnancy and delivery. Services Provided by a Gynecologist Preventive Care and Screenings Routine pelvic exams Pap smear and HPV testing for cervical cancer Breast examinations and mammography referrals STI screenings Contraceptive counseling and prescriptions Vaccinations including HPV, rubella Diagnosis and Treatment Menstrual irregularities (heavy, painful, or absent periods) Infections (vaginal, pelvic) Hormonal disorders like PCOS or thyroid problems Uterine fibroids, ovarian cysts, endometriosis Cancers of the reproductive organs Infertility assessment and management Pregnancy and Childbirth Care Preconception counseling Antenatal visits and monitoring Pregnancy complications management Delivery and postpartum care Surgical Procedures Minor: Pap smears, biopsies, IUD insertions Major: Laparoscopy, hysterectomy, cesarean sections What to Expect During a Gynecological Visit? Medical and menstrual history discussion Physical exam including breast and pelvic exam Possible diagnostic tests: ultrasound, Pap smear, blood tests Personalized health advice and treatment plans When Should You Visit a Gynecologist? Onset of menstruation or puberty Painful, irregular, or heavy periods Unusual vaginal discharge or odor Pelvic pain or pain during intercourse Planning for pregnancy or fertility issues Menopause symptoms Routine annual check-ups Common Myths About Gynecologists Myth Fact Pap smear is painful Usually causes mild discomfort, never extreme pain HPV vaccine means no more Pap smears Screening is still needed as vaccine doesn’t cover all HPV types Menopausal women don’t need checkups Postmenopausal screening is essential for continued cancer risk Gynecological visits in Pune are only for sexual health They cover comprehensive women’s health at all life stages FAQs At what age should girls see a gynecologist? Typically between ages 13-15 or soon after menstruation starts. Early visits focus on education and menstrual health. How often should women get a gynecological check-up? Most women should be seen annually or as recommended based on age, risk, and symptoms. Is an internal exam always needed during the first gynecologic visit? Not necessarily. For young or asymptomatic patients, the first visit may involve education and discussion without an internal exam.
Pelvic Inflammatory Disease (PID): Symptoms, Risks, and Treatment
Pelvic Inflammatory Disease (PID) is a common yet often underdiagnosed and misunderstood health issue affecting millions of women across India. Its impacts range from mild discomfort to severe reproductive complications, including fertility loss and chronic pelvic pain. This comprehensive blog sheds light on what PID is, how to recognize the symptoms, identify risk factors specific to Indian women, and understand the latest treatment approaches for effective management and prevention. What Is Pelvic Inflammatory Disease (PID)? PID is an infection of the female reproductive organs—including the uterus, fallopian tubes, and ovaries—primarily caused by sexually transmitted bacteria ascending from the vagina or cervix. If untreated, PID can cause pelvic adhesions, chronic pain, and increase the risk of ectopic pregnancies. Common Symptoms of PID Lower abdominal or pelvic pain, which may be mild to severe Heavy, foul-smelling, or unusual vaginal discharge Painful or difficult urination Pain during sexual intercourse Irregular menstrual bleeding or spotting Fever, chills, and nausea in severe infection Fatigue and general malaise Note: Some women, especially in early or mild PID, may show minimal or no symptoms, making screening and awareness critical. Risk Factors for Pelvic Inflammatory Disease in India Multiple sexual partners or unprotected sex History of sexually transmitted infections (STIs) such as chlamydia or gonorrhea Use of intrauterine devices (IUDs), especially soon after insertion without follow-up Early age of sexual activity or sexual abuse Poor genital hygiene or recurrent bacterial vaginosis Previous episodes of PID or pelvic surgery Lack of awareness and limited access to early screening and treatment Diagnosis and Testing Detailed medical and sexual history Pelvic examination: checking for cervical motion tenderness and adnexal tenderness Lab tests: vaginal/cervical swabs, STI screening, complete blood count Ultrasound to detect an abscess or inflammation Laparoscopy in uncertain or severe cases for direct visualization Treatment of PID Antibiotic therapy: Broad-spectrum antibiotics initiated promptly to cover likely bacterial causes, often continued for 14 days. Pain relief: NSAIDs and supportive care. Hospitalization: For severe cases, intravenous antibiotics and surgical drainage as needed. Partner treatment: Simultaneous STI treatment for sexual partners to prevent reinfection. Follow-ups: To ensure infection resolution and manage complications like infertility or chronic pain. Complications of Pelvic Inflammatory Disease Chronic pelvic pain due to adhesions or scarring Infertility from damaged fallopian tubes (leading cause in India) Increased risk of ectopic pregnancy, a medical emergency Recurrent PID episodes with progressive damage Preventive Measures Consistent use of condoms during sexual intercourse Regular screening for STIs in sexually active women Timely treatment of vaginitis or cervicitis Proper follow-up after IUD insertion Education and awareness programs, especially in rural or underserved communities Cultural and Social Factors in India Stigma around sexual health often delays care-seeking. Lack of open communication with healthcare providers may lead to untreated infection. Women’s empowerment and health education are critical to reducing PID burden. FAQ Can PID be cured completely? Early and proper treatment cures the infection and prevents most complications, but delayed treatment can cause permanent damage to reproductive organs. If I have mild pelvic discomfort, should I get tested for PID? Yes, especially if accompanied by abnormal discharge or fever. Early diagnosis improves outcomes. Are there home remedies for PID? No. PID requires medical treatment. Home remedies may relieve symptoms but do not treat the underlying infection.
High-Risk Pregnancy: What Does “High-Risk” Actually Mean?
A pregnancy is labeled “high-risk” when the mother, baby, or both face problems that could affect pregnancy outcomes—sometimes from the start, sometimes emerging along the way. This does not guarantee problems, but does mean extra vigilance and specialized antenatal care are needed. Common Causes in India Maternal Age: Under 18 or over 35 years old Medical Conditions: Hypertension, diabetes, thyroid problems, asthma, epilepsy, kidney or heart diseases Previous Obstetric History: Miscarriages, stillbirth, early labor, c-sections, complicated previous pregnancies Pregnancy Complications: Pre-eclampsia, gestational hypertension/diabetes, placenta previa/accreta Multiple Pregnancies: Twins, triplets Lifestyle Factors: Smoking, alcohol, high BMI, undernutrition Low Resources or Delayed Antenatal Care: Especially in rural India High-Risk Pregnancy: Key Statistics in India Nearly 40% of pregnant Indian women face one or more high-risk indicators. Complications are a leading cause of maternal and newborn deaths—most preventable with better monitoring and awareness. Social change (late marriage, focus on careers, fertility treatments) is leading to more first pregnancies after age 35. Monitoring: How is a High-Risk Pregnancy Followed? Frequent Doctor Visits: Monthly to every 2 weeks in early pregnancy; weekly or more in the last trimester for at-risk mothers Lab Tests: Blood count, blood sugar (fasting, post-meal, HbA1c) Thyroid profile, urine protein, liver/kidney function Infection screens, iron, and vitamin levels Ultrasonography and Imaging: First-trimester scan, anomaly scan (around 18-20 weeks), growth scans, and Doppler studies for baby’s well-being Assessment of placenta location and amniotic fluid Specialist Input: Cardiologist/endocrinologist/nephrologist as required Nutritionist/dietitian for meal plans in diabetes or preeclampsia Fetal Surveillance: Kick counts, non-stress tests (NST), and biophysical profiles in late pregnancy Prevention: Can High-Risk Pregnancies Be Avoided? Not all can be prevented, but risks drop dramatically with: Early, consistent prenatal care (antenatal registration ASAP) Optimal physical health before conception—manage blood pressure, sugar, weight, thyroid Avoiding smoking/alcohol, exposure to toxic chemicals Preconception vitamins (folic acid, iron) Managing Common High-Risk Scenarios 1. Hypertension and Preeclampsia Monitor BP at home, record all readings, report any swelling, headaches, or vision changes Reduce salt in diet Rest (side-lying) as needed Medications safe for blood pressure in pregnancy (as per doctor) 2. Gestational Diabetes Regular glucose monitoring, targeted diet plan with dietitian Exercise (walking, yoga); medicine or insulin if needed Monitor baby growth and avoid overdue pregnancies 3. Thyroid Disorders Strict medicine adherence, regular thyroid function tests Adjust dose every trimester as needed 4. Multiple Pregnancy More frequent scans, nutrition support (protein/iron/calorie needs go up) Monitoring for preterm labor Planning for possible NICU 5. Previous Loss or Preterm Birth Earlier, more intensive monitoring Cervical length measurement, possibility of progesterone or cerclage stitch Lifestyle & Home Care: What Indian Families Should Do Balanced nutrition: High-protein, iron, calcium, folate, fresh seasonal fruits/veggies; limit processed food Routine activity: Light household work, walking, and prenatal yoga (doctor approved) Rest: Nap/rest when tired, adjust work schedule as needed Mental health: Share worries, ask for help, join prenatal groups or WhatsApp support circles Managing Hospital Stays Some high-risk pregnancies require brief or extended hospital admission—for observation, medication, or delivery planning. Early communication can help mothers and caregivers plan support and finances. Delivery: When and How? Vaginal delivery is possible in many high-risk scenarios if the mother and baby are stable; C-section is planned for placenta previa, twin A breech, severe hypertension, or baby distress. Delivery is planned in a higher-level facility with blood bank and NICU access. Postpartum Considerations Monitor BP, sugar, and thyroid post-delivery—complications can persist or emerge Watch baby for feeding, color, activity; early gynecologist checkups are key Family/friend support for household duties and mother’s rest FAQ Can I have a safe and healthy baby if my pregnancy is high-risk? Absolutely—most high-risk pregnancies have healthy outcomes with early detection, regular monitoring, and close teamwork between mother, family, and doctors. What should I pack/prepare for more frequent hospital visits or a possible early delivery? Essential documents (ID, test records), phone chargers, small snacks, maternity clothes, baby basics, sanitary pads, and family support contacts. Can I work or travel during a high-risk pregnancy? It depends on your risk type and doctor’s advice. Most mothers can do light work and moderate activity. Long travel, night shifts, and standing for hours may need to be restricted.
Female Infertility: Common Causes and When to Seek Help
Infertility affects millions of couples across India, often silently disrupting hope and emotional well-being. Around one in six couples struggle to conceive, and in nearly half of those cases, female factors contribute either partly or entirely. Female infertility isn’t just about inability—it’s about timing, ovulation, hormones, lifestyle, and sometimes complex underlying conditions. The good news is that with modern diagnostics and treatment, more women today are becoming mothers than ever before. This blog unpacks the causes, symptoms, and treatments for female infertility, alongside when you should seek help. It also highlights the importance of early evaluation, realistic expectations, and understanding that infertility is a medical condition—not a stigma. Understanding Infertility Definition: Female infertility refers to the inability to conceive after one year of regular unprotected sexual activity (or six months if the woman is 35 or older). It can result from hormonal, structural, or functional issues. Sometimes, multiple causes coexist—or no clear reason is ever found (unexplained infertility). Common Causes of Female Infertility 1. Ovulation Disorders The most frequent cause of female infertility. Ovulation means the release of a mature egg from the ovary each month. Common conditions: Polycystic Ovary Syndrome (PCOS): The leading cause in Indian women, resulting in irregular periods, excessive hair growth, and weight changes. Hormonal Imbalance: Issues in the hypothalamus or pituitary gland can disrupt reproductive hormones. Premature Ovarian Failure (POF): Early depletion of eggs before age 40, sometimes with family history or autoimmune link. Thyroid Disorders: Both hyperthyroidism and hypothyroidism can affect ovulation. Excessive Stress or Exercise: Can suppress menstruation temporarily, disrupting ovulation cycles. 2. Tubal Blockage or Damage The fallopian tubes carry eggs to meet sperm for fertilization. Damage or scarring blocks the path. Causes include: Pelvic Inflammatory Disease (PID) Untreated sexually transmitted infections (STIs) Previous surgeries like appendectomy or C-section Endometriosis causing scarring or adhesions 3. Uterine or Cervical Abnormalities Structural problems can prevent implantation or increase miscarriage risk. Examples: Uterine fibroids or polyps Congenital defects such as septate uterus Scar tissue from previous surgery (Asherman’s syndrome) Abnormal cervical mucus (can hinder sperm movement) 4. Endometriosis Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus. It can cause inflammation, pain, and damage to reproductive organs. Around 25–40% of women with infertility have this condition. 5. Age-related Decline Women are born with a finite supply of eggs, which diminishes in both quantity and quality with age—sharper after 35. Older eggs have higher chances of chromosomal abnormalities, making conception and healthy pregnancy harder. 6. Unknown (Unexplained) Infertility In about 10–15% of couples, no visible causes are identified despite all tests being normal. Subtle hormonal, immune, or implantation factors may be at play. When to Seek Help You don’t have to wait endlessly or guess if conception delays. Here’s when it’s time to consult a fertility specialist: Age When to see a specialist < 35 years After 1 year of trying without success 35–39 years After 6 months 40+ years Immediately or after 3 months Also seek help if you have: Irregular or absent periods History of pelvic infection or surgery Diagnosed PCOS or thyroid/hormonal issues Known uterine abnormalities or painful cycles Partner with known male fertility problems Diagnostic Tests for Female Infertility Doctors perform stepwise evaluation to uncover causes: Blood tests: Hormone levels (FSH, LH, AMH, prolactin, thyroid) Ultrasound: Identifies PCOS, fibroids, or ovarian reserve Hysterosalpingography: X-ray dye test to check fallopian tube openness Laparoscopy: Keyhole surgery to examine uterus, tubes, and ovaries directly Ovarian Reserve Tests: AMH test for egg supply Proper diagnosis avoids guesswork and guides effective treatment. Treatment Options Modern infertility care in India offers a wide range of the latest therapies: 1. Lifestyle and Natural Optimization Weight management for PCOS or obesity-related infertility Balanced diet rich in protein, iron, vitamins Regular moderate exercise, stress reduction, yoga Avoid tobacco, alcohol, and excessive caffeine 2. Medications Ovulation induction: Medicines like clomiphene or letrozole to stimulate eggs Hormone therapies: Correct thyroid or prolactin disorders Metformin: For insulin resistance in PCOS 3. Surgical Intervention Laparoscopic removal of fibroids, polyps, or endometriotic lesions Tubal reconstructive surgeries if blocked Correction of uterine septum or adhesions 4. Assisted Reproductive Technology (ART) Indian fertility centers now provide best-in-class solutions: IUI (Intrauterine Insemination): Processed sperm placed directly in uterus. IVF (In Vitro Fertilization): Eggs and sperm combined outside then implanted. ICSI (Intracytoplasmic Sperm Injection): A single sperm injected into egg—useful for low sperm count. Egg freezing / Donor eggs: Options for women with reduced egg reserve or career priorities. Surrogacy: Considered legally and medically for specific cases. 5. Psychological Counseling and Support Fertility journeys often bring stress, guilt, or relationship strain. Emotional well-being contributes significantly to treatment success. Support groups, therapy, or guidance sessions are recommended in parallel with medical care. Preventing Female Infertility: Practical Tips Schedule regular gynecological checkups. Treat UTIs, pelvic infections, or STIs early. Maintain a normal BMI; obesity reduces fertility success rates. Track ovulation to understand fertile window. Avoid overuse of emergency contraceptives. Get evaluated before age 35 if planning to delay pregnancy. Vaccinate for rubella and HPV as advised. Infertility in India: The Social Perspective In India, female infertility still carries stigma, but societal understanding is improving. With access to reproductive specialists even beyond metros, modern couples now prioritize early diagnosis and evidence-based treatment. From working professionals using IVF to couples opting for genetic screening, the field is evolving rapidly—and success rates continue to rise. FAQ Is female infertility always permanent? No. Many causes like hormonal imbalance, PCOS, and mild endometriosis are treatable. Even women with complex issues can conceive with Assisted Reproductive Technology (ART). Early evaluation is the key to success. Can lifestyle really affect fertility that much? Absolutely. Being overweight or underweight, smoking, excess alcohol, unmanaged stress, and lack of exercise all disturb hormonal balance and ovulation. Adopting a healthy routine can naturally enhance fertility potential. I’m over 35—should I panic? No need to panic, but do act proactively. Egg count and quality decline with time, so timely consultation with a fertility specialist is recommended. Options like IVF
Heavy Menstrual Bleeding (Menorrhagia): When Is It a Serious Problem?
Menstruation is a normal part of every woman’s reproductive health, but when periods become unusually heavy or prolonged, they may signal an underlying medical condition. Heavy menstrual bleeding, medically referred to as menorrhagia, is defined as excessive blood loss during periods that interferes with daily life. In India, this condition often goes unreported because many women consider heavy periods “normal” or hesitate to discuss menstrual health openly. However, untreated menorrhagia can lead to anemia, severe fatigue, and in some cases, reveal more serious gynecological issues. Understanding its symptoms, causes, and treatment options is critical for women of all ages. What is Menorrhagia? Menorrhagia is not about slightly heavier flow—it is a condition where periods are abnormally heavy or extended. A normal period usually lasts 4–7 days with a manageable flow. With menorrhagia, bleeding may: Last longer than a week. Require frequent change of sanitary pads (every 1–2 hours). Be accompanied by blood clots larger than a coin. Cause disruption of daily life due to excessive bleeding and exhaustion. Common Symptoms of Heavy Menstrual Bleeding Heavy menstrual bleeding isn’t just about quantity—it also affects overall health and comfort. Soaking through pads/tampons within an hour, repeatedly. Needing double sanitary protection during periods. Passing clots larger than 2.5 cm in diameter. Feeling tired, weak, or dizzy during and after periods. Shortness of breath due to low hemoglobin. Painful cramps that worsen with heavy blood loss. If any of these symptoms occur regularly, it is important to seek professional medical evaluation. Causes of Menorrhagia Multiple factors can contribute to abnormal uterine bleeding. Some are temporary, while others may need medical treatment. 1. Hormonal Imbalance In reproductive age, estrogen and progesterone imbalance can lead to thickening of the uterine lining, causing heavier bleeding. Common in adolescents after menarche and in women approaching menopause. 2. Uterine Fibroids and Polyps Non-cancerous growths in the uterus often lead to heavy, longer periods. Indian women in their 30s and 40s are especially prone. 3. Gynecological Conditions Adenomyosis: Uterine lining tissue growing into the muscle wall. Endometriosis: Tissue similar to uterine lining growing outside the uterus. 4. Medical Disorders Thyroid imbalance, blood clotting disorders, or liver disease can worsen bleeding. 5. Pregnancy-Related Issues Miscarriage or ectopic pregnancy may present as unusually heavy bleeding. 6. Medications Certain blood thinners, hormonal treatments, and intrauterine contraceptive devices (IUDs) can cause increased flow. When to Worry: Red Flags Heavy bleeding becomes a serious health concern when: It consistently disrupts work, school, or social life. There are signs of anemia—extreme fatigue, paleness, or breathlessness. Clots are very large and frequent. Bleeding occurs in between cycles. The age factor is high—women nearing menopause or those who recently started menstruating should pay careful attention. Prompt medical consultation is essential in these cases to avoid long-term complications. Diagnosis of Heavy Menstrual Bleeding Doctors may recommend certain tests to confirm the cause: Medical history and pelvic exam Blood tests (to check for anemia, thyroid issues, clotting disorders) Ultrasound of the uterus and ovaries Endometrial biopsy in some women (especially over 40 years) Pap smear or hysteroscopy if abnormal cells or growths are suspected Treatment Options for Menorrhagia The treatment depends on the cause, age, severity, and whether a woman wishes to have children in the future. 1. Medications Tranexamic acid: Helps reduce bleeding. NSAIDs (like ibuprofen): Reduce both pain and bleeding. Hormonal therapy: Pills, patches, IUDs, or injections to regulate cycles. Iron supplements: To correct anemia caused by blood loss. 2. Surgical Procedures D&C (Dilation and Curettage): Temporary relief by scraping uterine lining. Endometrial ablation: Destruction of uterine lining to reduce bleeding. Uterine fibroid removal (myomectomy). Hysterectomy (removal of uterus): Permanent solution in severe, unmanageable cases. Lifestyle Changes to Support Healthy Periods Along with treatment, lifestyle adjustments make a big difference in reducing symptoms. Maintain a balanced diet rich in iron (green leafy vegetables, jaggery, dates, pulses). Hydration helps manage headaches and weakness. Practice yoga and breathing exercises to reduce stress-related menstrual irregularities. Keep a menstrual diary to track patterns, flow, and any warning signs. Avoid smoking, excessive caffeine, and junk food that worsen cramps and fatigue. Heavy Menstrual Bleeding in India: The Cultural Challenge In India, many women normalize heavy periods or avoid seeking treatment due to stigma or lack of awareness. Social discomfort, myths, and hesitation in discussing menstrual health further delay diagnosis. Regular gynecological check-ups and awareness about treatment options can prevent women from silently suffering. Empowering women through education about when bleeding is too heavy and encouraging open conversations is a vital step towards better reproductive health outcomes across communities. FAQ Is heavy menstrual bleeding always a sign of a serious problem? Not always. Sometimes lifestyle changes or minor hormonal shifts can cause temporary heavy bleeding. However, if it continues for more than two cycles or is associated with severe pain and anemia, it requires evaluation. Can diet reduce heavy periods? Diet alone cannot treat menorrhagia, but eating iron-rich foods can help prevent complications like anemia. Nutritional support can also make medical treatments more effective. When should teenagers be concerned about heavy bleeding? Adolescent girls may have irregular heavy cycles initially due to hormonal immaturity. But if bleeding is excessive, disrupts daily life, or causes weakness, parents should consult a doctor to rule out conditions like clotting disorders or hormonal imbalance.
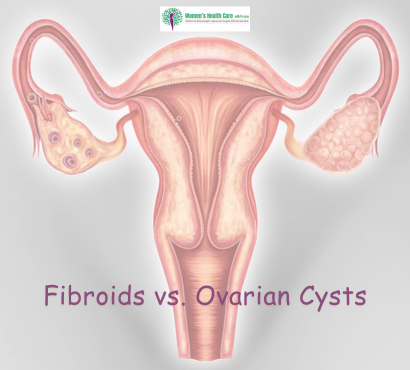
Fibroids vs. Ovarian Cysts: Differences, Symptoms, and Treatment
Women’s reproductive health is complex, and two common conditions that often cause confusion are fibroids and ovarian cysts. While both can affect fertility, menstrual cycles, and overall well-being, they are not the same. Understanding the differences, symptoms, and treatment options for fibroids and ovarian cysts is crucial for women to make informed healthcare decisions. aims to provide a comprehensive guide to distinguish between fibroids and ovarian cysts, their causes, risk factors, and available treatments. What Are Fibroids? Fibroids, also called uterine leiomyomas or myomas, are non-cancerous growths that develop within the uterus (womb). They are made up of muscle tissue and fibrous tissue and vary in size—from as small as a seed to as large as a melon. Key Characteristics of Fibroids: Origin: Inside or on the wall of the uterus. Nature: Solid, firm growths. Growth: Hormone-dependent, especially influenced by estrogen and progesterone. Common Age Group: Most common in women aged 30–50 years. What Are Ovarian Cysts? Ovarian cysts are fluid-filled sacs that develop inside or on the surface of the ovaries. Unlike fibroids, they are usually soft and filled with fluid. Many cysts are harmless and resolve on their own, but some may cause problems. Key Characteristics of Ovarian Cysts: Origin: Inside or outside the ovary. Nature: Fluid-filled, sometimes containing tissue or blood. Growth: Often linked to the menstrual cycle or conditions like polycystic ovary syndrome (PCOS). Common Age Group: Can affect women of all ages, especially during reproductive years. Major Differences Between Fibroids and Ovarian Cysts Feature Fibroids Ovarian Cysts Location Uterus (womb) Ovaries Composition Solid muscle and fibrous tissue Fluid-filled sac (sometimes mixed tissue) Growth Factor Hormone-dependent (estrogen, progesterone) Often related to ovulation or PCOS Symptoms Heavy bleeding, pelvic pain, infertility Bloating, irregular periods, pain Treatment Medication, surgery (myomectomy, hysterectomy) Observation, hormonal therapy, surgery if large Symptoms of Fibroids Fibroids may be symptomless in some women, but when symptoms occur, they can include: Heavy or prolonged menstrual bleeding Pelvic pain or pressure Enlarged abdomen or bloating Frequent urination (due to pressure on the bladder) Constipation (if pressing on the rectum) Painful intercourse Difficulty conceiving or pregnancy complications Symptoms of Ovarian Cysts Ovarian cysts also vary in presentation. Many small cysts go unnoticed, but larger or persistent ones may cause: Pelvic pain (sharp or dull) Bloating or abdominal swelling Pain during sex Irregular menstrual cycles Nausea or vomiting (if cyst ruptures) Difficulty emptying the bladder or bowel Sudden severe pain (if the cyst twists the ovary – ovarian torsion) Causes and Risk Factors Causes of Fibroids: Hormonal imbalance (high estrogen and progesterone) Genetics (family history of fibroids) Lifestyle factors (obesity, high red meat intake, low vitamin D levels) Early onset of menstruation Causes of Ovarian Cysts: Ovulation (follicle that doesn’t release an egg may turn into a cyst) Hormonal problems Polycystic ovary syndrome (PCOS) Pregnancy (cysts may form early and usually resolve) Severe pelvic infections spreading to ovaries Diagnosis of Fibroids and Ovarian Cysts Fibroids Diagnosis: Ultrasound scan (pelvic ultrasound) MRI (for detailed imaging) Hysteroscopy (camera inserted into uterus) Ovarian Cysts Diagnosis: Ultrasound scan (transvaginal or abdominal) Blood tests (to check hormone levels, CA-125 for cancer risk) CT or MRI scans (in complex cases) Treatment Options Treatment for Fibroids: Medications: Hormonal therapy (birth control pills, GnRH agonists) Tranexamic acid for heavy bleeding Minimally invasive procedures: Uterine artery embolization (blocks blood flow to fibroids) Radiofrequency ablation Surgical treatment: Myomectomy (removal of fibroids, preserving uterus) Hysterectomy (complete removal of uterus in severe cases) Treatment for Ovarian Cysts: Observation: Many cysts shrink naturally. Medications: Birth control pills to regulate ovulation. Surgery (if large, persistent, or cancerous risk): Laparoscopy (keyhole surgery to remove cysts) Laparotomy (for larger or suspicious cysts) Can Fibroids and Ovarian Cysts Affect Fertility? Yes, both conditions may impact fertility. Fibroids: Large fibroids can block fallopian tubes or distort the uterine cavity, making conception difficult. Ovarian Cysts: Conditions like PCOS lead to irregular ovulation, affecting fertility. Early detection and treatment can significantly improve chances of conception and healthy pregnancy. Lifestyle and Home Care Tips Maintain a balanced diet rich in fruits, vegetables, and whole grains. Exercise regularly to maintain a healthy weight. Avoid excess alcohol and processed foods. Manage stress (yoga, meditation). Schedule regular gynecological check-ups for early detection. FAQs 1. Can fibroids turn into cancer? No, fibroids are non-cancerous. In very rare cases (<1%), they may develop into a cancerous tumor called leiomyosarcoma. 2. Do ovarian cysts always need surgery? No. Most ovarian cysts disappear on their own within a few menstrual cycles. Surgery is needed only if they are large, painful, or suspicious of cancer. 3. Can fibroids or cysts come back after treatment? Yes. Fibroids may regrow after treatment if the uterus is preserved. Ovarian cysts may recur due to hormonal cycles or PCOS. Regular monitoring helps in long-term management.