Cervical cancer is one of the most common cancers affecting women worldwide, but it is also one of the most preventable. In India, cervical cancer accounts for a significant number of cancer cases among women, particularly in the 30–50 age group. The good news? Early detection and preventive measures — including the HPV vaccine — can dramatically reduce the risk. the early signs, the importance of screening, and how vaccination can help in prevention. What Is Cervical Cancer? Cervical cancer occurs in the cells of the cervix — the lower part of the uterus that connects to the vagina. Most cases are linked to persistent infection with high-risk types of the Human Papillomavirus (HPV), a common sexually transmitted infection. While HPV infection is common, it doesn’t always lead to cancer. In many women, the body’s immune system clears the virus naturally. However, in some cases, the infection persists, causing abnormal cell changes that can develop into cancer over time. Early Signs and Symptoms of Cervical Cancer Cervical cancer often develops slowly, and early stages usually do not present obvious symptoms. This is why screening is critical. However, in more advanced stages, you may notice: Abnormal vaginal bleeding — after intercourse, between periods, or after menopause Unusual vaginal discharge — watery, bloody, or with a foul odor Pelvic pain or pain during intercourse Longer or heavier menstrual periods Important: These symptoms can also be caused by other conditions, but it’s best to consult a gynecologist promptly. Risk Factors for Cervical Cancer While HPV infection is the primary cause, other factors can increase your risk: Early sexual activity or multiple sexual partners Weak immune system (HIV, long-term immunosuppressive therapy) Smoking Long-term use of oral contraceptives (over 5 years) Multiple full-term pregnancies Lack of regular screening The Role of Screening in Early Detection Screening can detect precancerous changes before they turn into cancer. In India, Pap smears and HPV DNA tests are the two primary screening methods. 1. Pap Smear Test Detects abnormal cell changes in the cervix Recommended every 3 years for women aged 21–65 Can be combined with an HPV test for more accuracy 2. HPV DNA Test Detects high-risk HPV strains that can cause cervical cancer Recommended every 5 years for women aged 30 and above, along with a Pap test Tip: Even if you’ve received the HPV vaccine, regular screening is still necessary. HPV Vaccine: Your Best Preventive Weapon The HPV vaccine protects against the most common cancer-causing HPV types (16 and 18), which are responsible for around 70% of cervical cancer cases. Some vaccines also protect against HPV types causing genital warts. Who Should Get the HPV Vaccine? Girls and women aged 9–26 years benefit most when vaccinated before sexual activity begins Can also be given to women up to age 45 after discussing with a doctor Boys can also be vaccinated to reduce HPV transmission Types of HPV Vaccines Available in India Cervarix – protects against HPV types 16 and 18 Gardasil – protects against HPV types 6, 11, 16, and 18 Gardasil 9 – protects against nine HPV types (not yet widely available in India) Dosage: For ages 9–14: Two doses, 6–12 months apart For ages 15+: Three doses over 6 months Prevention Tips Beyond Vaccination Practice safe sex (use condoms) Avoid smoking Maintain a healthy immune system through proper diet, exercise, and sleep Get regular gynecological check-ups and screenings Educate women and young girls about HPV and cervical cancer risks Why Awareness Matters in India In India, many women are diagnosed at advanced stages due to lack of awareness and limited access to screening. Social stigma and myths about gynecological exams also delay diagnosis. Public health campaigns and open conversations are vital to encourage timely screening and vaccination. Cervical cancer is highly preventable through early detection, vaccination, and lifestyle choices. By combining HPV vaccination with regular screening, women can significantly lower their risk. Knowledge, awareness, and timely action can save thousands of lives every year. FAQs Can cervical cancer be completely cured if detected early? Yes. When detected in its early stages, cervical cancer has a high cure rate with appropriate treatment. Do I still need a Pap smear if I have received the HPV vaccine? Yes. The vaccine does not protect against all HPV types, so regular screening is still essential. Is the HPV vaccine safe? Yes. It is approved by health authorities worldwide and has been proven safe and effective with minimal side effects like mild fever or injection site pain.
Common Gynecological Problems Every Woman Should Know About
1. Why Awareness Matters Gynecological health significantly influences a woman’s physical, emotional, and social wellbeing. Many conditions—PCOS, menstrual disorders, infections—are often misunderstood, stigmatized, or overlooked. Raising awareness empowers timely care, preventing complications like infertility or chronic pain. Open dialogue starts with recognizing and addressing common issues. 2. Irregular Periods: When “Normal” Isn’t Clear What It Means A normal menstrual cycle ranges from 21 to 35 days. Irregular periods include: Skipped or missed cycles Heavy or unusually light flow Cycles shorter than 21 days or longer than 35 Common Causes Hormonal shifts (adolescence, perimenopause) PCOS imbalance Stress or rapid weight changes Thyroid abnormalities Uterine fibroids or polyps Red Flags Very heavy flow (soaking >1 pad/hour) Bleeding after menopause or between cycles Persistent irregularities affecting daily life Self-Care Tips Track cycles with apps or journals Maintain balanced diet and weight Manage stress with yoga, mindfulness Exercise moderately to support hormonal balance 3. PCOS (Polycystic Ovary Syndrome) Symptoms Irregular periods or skipped cycles Excess facial/body hair (hirsutism) Acne or oily skin Weight gain, especially around the abdomen Small ovarian cysts seen in scans Why It Happens Insulin resistance stimulates excess androgens, disrupting ovulation and causing cyst formation. Health Impacts Infertility or delayed conception Higher risk of diabetes, heart disease Sleep apnea and liver issues (NAFLD) Management Balanced, low-GI diet to regulate insulin Physical activity: brisk walking, strength training Stress reduction techniques Medications as prescribed by professionals 4. Urinary & Vaginal Infections A. Bacterial Vaginosis (BV) & Yeast Infections Yeast Infections Thick white discharge with itching Worsens after antibiotics or in hot, humid climates BV Thin, greyish discharge with fishy odor Often associated with unprotected sex or wiping habits B. Urinary Tract Infections (UTIs) Burning sensation during urination Sudden urge to urinate with minimal output Lower abdominal pain Prevention Wipe front-to-back Change wet clothes promptly Stay hydrated Avoid scented feminine products 5. Uterine Fibroids & Endometriosis A. Uterine Fibroids Non-cancerous muscle growths in the uterus Symptoms: heavy bleeding, pelvic pain, pressure on bladder/bowels B. Endometriosis Tissue resembling uterine lining grows outside the uterus Causes severe cramps, painful intercourse, infertility Self-Awareness Track symptoms: heavy flow, pelvic pain, painful sex Acknowledge when menstrual pain is more than “just cramps” 6. Pelvic Pain & Prolapse Issues Chronic Pelvic Pain Lasts >6 months May be caused by pelvic inflammatory disease (PID), scarring, or adhesions Pelvic Organ Prolapse Uterus, bladder, or rectum descends into the vaginal canal Symptoms: heaviness, urinary or bowel trouble, sexual discomfort Self-Management Pelvic floor strengthening (Kegels, pelvic physiotherapy) Avoid heavy lifting Maintain healthy weight 7. Cycle-Related Anemia & Iron Deficiency Heavy bleeding or prolonged periods can deplete iron stores, leading to fatigue, pallor, and dizziness. Self-Support Eat iron-rich foods (spinach, pulses, lean meat) Pair with vitamin C for better absorption Periods exceeding 7 days warrant medical attention 8. Breast Self-Exams & Awareness While not strictly gynecological, breast health is linked to reproductive hormones. How to Examine Monthly self-checks in the shower or in front of a mirror Feel for lumps or asymmetry Report any unusual signs like nipple discharge or skin puckering 9. When to Seek Medical Guidance Any of the following warrant professional evaluation: Heavy flow impairing daily life Sudden unexplained pelvic or abdominal pain Suspected infections Issues with fertility or recurring cycles Suspected prolapse symptoms Early action ensures better outcomes. 10. Self-Care Routine: A Week in the Life Day Action Any Drink 2–3 L water • Practice pelvic floor exercises Menses Track flow and mood • Replenish iron nutrients Weekly Check for unusual discharge or odor Monthly Perform breast self-exam • Note menstrual changes Occasionally Practice yoga/stretching for pelvic health Understanding your body is the first act of empowerment. By recognizing common gynecological issues—from irregular cycles to pelvic pain—you build confidence to take charge and seek help early. A gentle habit of tracking cycles, practicing pelvic awareness, and paying attention to warning signs fosters not only physical health, but emotional resilience too. FAQs Q1. How do I know if my periods are unusually heavy? Fufilling a pad or tampon every 1–2 hours or passing clots larger than a quarter suggests heavy bleeding—talk to a healthcare provider. Q2. Can PCOS be reversed naturally? Lifestyle changes—balanced diet, regular exercise, stress management—can significantly improve or reverse PCOS symptoms over time. Q3. Do yeast infections need medication? Mild infections may respond to over-the-counter treatments, but recurrent or severe cases warrant a check-up for confirmation and tailored care.
Polycystic Ovary Syndrome (PCOS): Symptoms, Diagnosis, and Management
Polycystic Ovary Syndrome (PCOS) is a complex hormonal disorder affecting an estimated 3.7–22.5% of Indian women, causing irregular menstruation, high androgens, and problems with metabolism and fertility. Lifestyle changes and early diagnosis pave the way for improved long-term health. 2 | What Is PCOS? A multifactorial condition characterized by: Hormonal imbalance: elevated androgens (testosterone) Menstrual irregularity: absent, scarce, or unpredictable periods Polycystic ovaries: many small follicles visible on ultrasound Often accompanied by insulin resistance, central obesity, acne, excess body hair, infertility, and mood issues. 3 | Key Symptoms Symptom What to Look For Periods <9 cycles/year, >35 days apart, or absent for 3+ months Hyperandrogenism Facial hair, scalp hair thinning, and moderate-to-severe acne Weight Gain Central/abdominal obesity (waist >80 cm); >40% obese among Indian women with PCOS. Skin Changes Dark underarms/neck patches (acanthosis nigricans) Infertility Difficulty conceiving due to irregular ovulation Insulin Resistance Cravings, fatigue, family history of diabetes Emotional Impact Anxiety, depression, body image issues 4 | Diagnosis Criteria PCOS diagnosis requires 2 of the following 3, with other causes excluded (Rotterdam criteria) Irregular/anovulatory cycles Clinical or lab evidence of high androgens Polycystic ovaries (≥12 follicles 2–9 mm) on ultrasound Additional tests may include thyroid, prolactin levels, and adrenal function to rule out other disorders. 5 | Role of Insulin Resistance & Hormones Insulin resistance is central to PCOS—it increases insulin, which signals the ovaries to produce more testosterone. Genetic predisposition and lifestyle factors like weight and diet are both contributors. 6 | Management Approaches A. Lifestyle First Weight management: Losing 5–10% body weight can restore ovulation and improve insulin sensitivity Balanced diet: Low-glycemic carbs, high fiber, lean protein, omega-3s, along with superfoods like chickpeas, cinnamon, jambul, moringa for blood sugar control as per Indian nutrition insights Regular exercise: 150 minutes/week helps menstrual regulation and metabolic health B. Medication Metformin to reduce insulin resistance Hormonal contraceptives to regulate cycles and reduce androgens Anti-androgens like spironolactone for acne and hair growth Ovulation induction (letrozole, clomiphene) for pregnancy C. Supplements & Adjuncts Myo-inositol to improve ovulation and hormone markers Vitamin D and probiotics may aid metabolic and hormonal balance D. Addressing Emotional Wellness Psychological support is key—mood disorders are common due to hormonal imbalances and fertility challenges. E. Ongoing Monitoring Regular checks: weight/BMI, glucose, lipid profile, ultrasound for ovarian size 7 | Supporting Infertility Weight loss + ovulation medication resolves most cases If needed: IUI or IVF after 6–12 months of conservative therapy PCOS pregnancies are higher risk—must be monitored for gestational diabetes and hypertension 8 | Long-Term Health Risks Women with PCOS have elevated risks of: Type 2 diabetes Heart disease Dyslipidaemia Sleep apnea Anxiety and depression Ongoing care and screening are essential. 9 | When to Consult Seek evaluation if you experience: Irregular or missed periods for over 3 months Significant acne or sudden hair growth Weight gain with hunger or fatigue Difficulty conceiving after 6 months of trying Early diagnosis enables better long-term outcomes. PCOS affects many Indian women but can be skillfully managed with early detection, consistent lifestyle measures, tailored medications, and emotional support. Creating awareness and access to good care empowers women to enjoy vibrant reproductive and overall health. FAQs Q1: Can PCOS be cured? There is no cure, but symptoms can be managed effectively. With lifestyle changes and appropriate therapies, many women restore ovulation, manage weight, reduce acne, and conceive. Q2: What diet is best for PCOS? A low–moderate glycemic diet high in fiber, lean protein, healthy fats (like nuts and seeds), and anti-inflammatory foods supports hormonal balance and weight management. Q3: Can lean women get PCOS? Yes. While insulin resistance is common, thin women may still experience hormonal imbalance and irregular ovulation. Treatment is similar—prefer lifestyle, supplements, and ovulation support.
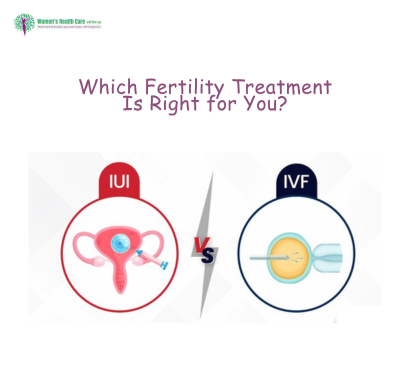
IUI vs. IVF: Which Fertility Treatment Is Right for You?
Infertility affects many couples today, and assisted reproductive technologies (ART) like Intrauterine Insemination (IUI) and In Vitro Fertilization (IVF) are widely used to increase chances of conception. Choosing between IUI and IVF is an important decision influenced by age, diagnosis, budget, and emotional resilience. Here’s an in-depth guide to help you evaluate which fits your journey. Understanding IUI vs IVF A. What is IUI? Sperm is washed and placed directly into the uterus during ovulation. Involves minimal intervention and stimulation. Best when mild male factor, unexplained infertility, or cervical issues are present. B. What is IVF? Ovarian stimulation, egg retrieval, fertilisation in the lab, and embryo transfer. Suitable for severe male factor, blocked tubes, advanced maternal age, or genetic screening. Step-by-Step Process Comparison IUI Steps: Ovarian monitoring via ultrasound. Mild hormonal stimulation (Clomid or injectables). Sperm preparation and timed intrauterine transfer. Pregnancy test after 2 weeks. IVF Steps: Full ovarian stimulation (hormone shots). Egg retrieval under sedation. Fertilisation in lab incubator. Embryo culture and selection. Transfer 1–2 embryos. Pregnancy test after 2 weeks. Success Rates & Factors Treatment Ideal Age Avg Success Rate IUI <35 10–20% per cycle IVF <35 40–50% per cycle 35–40 IVF: 20–30% Key Factors: Age and egg quality Sperm health Cause of infertility Lifestyle (BMI, diet, sleep) Emotional support Cost Comparison (India) Treatment Per Cycle Cost (INR) Additional Costs IUI ₹15,000–₹40,000 Medications ₹5–10k IVF ₹1,40,000–₹2,50,000 Medications ₹30k–₹60k Financial Tips: Start with IUI in mild cases before moving to IVF. Check package offers with medication included. Budget for 3–4 cycles to increase success chances. Risks & Considerations IUI: Mild side effects from hormone meds Risk of multiple pregnancy if multiple eggs released Minimal discomfort and convenience IVF: Hormonal side effects, ovarian hyperstimulation risk Invasive procedures: egg collection/pitocin Emotional and physical toll Risks like multiple pregnancy or procedure complications Who Should Choose Which? Choose IUI if: Age <35, unexplained infertility, mild male factor, ovulation issues. No severe tubal blockage. Choose IVF if: Bilateral tubal block, older age, poor sperm Previous IUI failures Genetic screening needed 👉 In many cases, doctors recommend trying 3 cycles of IUI before switching to IVF. Emotional and Physical Preparation Discuss therapy or support groups for the emotional toll Maintain healthy diet, exercise, manage stress Attend all follow-ups and understand procedures Choosing between IUI and IVF depends on fertility diagnosis, age, costs, and your emotional readiness. Starting with IUI can be less invasive and cost-effective. If unsuccessful, IVF offers higher success with more complexity. Work closely with your fertility specialist to design a personalized treatment path, and remember self-care and support matter as much as medical decisions. FAQs Q1. How many IUI cycles should I try before IVF? Typically 3–4 IUI cycles are recommended. If unsuccessful, then IVF is advised—especially for women over 35. Q2. Can IVF guarantee pregnancy? No guarantee—IVF success rates depend on multiple factors but currently hover at 40–50% per cycle in healthy young couples. Q3. Does BMI affect success rates? Yes—both overweight and severely underweight women face reduced success in IUI/IVF. A BMI of 18.5–24.9 is ideal for treatment.
Urinary Tract Infections (UTIs) in Women: Causes, Symptoms, and Prevention
Urinary Tract Infections (UTIs) are among the most common bacterial infections affecting women. In fact, research suggests that over 50% of women will experience at least one UTI in their lifetime, and many will face recurrent infections. While a UTI may seem like a minor issue, if left untreated, it can lead to serious health complications, including kidney infections. In this detailed blog, we explore everything you need to know about UTIs in women—causes, symptoms, prevention, and treatment—tailored to the Indian demographic and lifestyle context. What Is a UTI? A UTI (Urinary Tract Infection) is an infection caused by bacteria entering the urinary system, which includes: Urethra (urethritis) Bladder (cystitis) Ureters Kidneys (pyelonephritis) In women, the shorter urethra makes it easier for bacteria to reach the bladder, making UTIs more frequent. Causes of UTIs in Women Poor hygiene practices Wiping from back to front Not cleaning genital area properly after urination or defecation Sexual activity Intercourse can introduce bacteria into the urethra Holding urine for long periods Allows bacteria to multiply Use of irritants Harsh soaps, douches, or feminine hygiene sprays Dehydration Less urination leads to bacterial buildup Urinary tract abnormalities or blockages Kidney stones or an enlarged uterus during pregnancy Uncontrolled diabetes High sugar levels in urine encourage bacterial growth Common Symptoms Burning or pain while urinating Frequent urge to urinate, even after just going Cloudy, dark, or foul-smelling urine Pain in the lower abdomen or back Mild fever (in advanced cases) Fatigue or general discomfort When to See a Doctor Seek immediate medical attention if: Fever >101°F Blood in urine Nausea or vomiting Persistent back pain Recurrent UTIs (more than 2 in 6 months) Diagnosis Urine Analysis Checks for white blood cells, red blood cells, and bacteria Urine Culture Identifies the specific bacteria causing infection Ultrasound or CT scan In recurrent or complicated cases Treatment Options in India Antibiotics Common ones include nitrofurantoin, trimethoprim-sulfamethoxazole, and fosfomycin Pain relief Phenazopyridine for urinary discomfort Hydration therapy Drinking at least 2.5–3 liters of water daily Probiotic supplements Help restore good bacteria Note: Self-medication can be dangerous. Always consult a urologist or gynecologist. Home Remedies (Supportive, Not Curative) Cranberry juice: May prevent bacteria from adhering to bladder walls Tulsi leaves: Natural antibacterial properties Jeera (cumin) water: Reduces inflammation Curd (yogurt): Source of probiotics Prevention Tips for Indian Women Wipe front to back Avoid synthetic undergarments Pee after sex Don’t hold urine Use clean toilets when traveling Stay hydrated Limit sugary foods Avoid harsh feminine washes Special Considerations: UTIs During Pregnancy UTIs during pregnancy are more dangerous and can lead to: Preterm labor Low birth weight Kidney infection Routine screening is a must during prenatal visits. UTIs and Menopause Estrogen decline affects the vaginal and urinary flora, increasing infection risk. Local estrogen therapy can sometimes help post-menopausal women prevent UTIs. UTIs vs. Other Conditions Condition Similar Symptom Differentiating Factor UTI Burning urine Positive urine culture Vaginal infection Discomfort Vaginal discharge, itching Kidney stone Pain Sharp back pain, visible stone on scan Recurring UTIs Causes may include: Anatomical issues Diabetes Menopause Sexual activity Treatment may involve a long-term low-dose antibiotic plan or lifestyle changes. Cost of UTI Treatment in India (2025 Rates) Treatment Approximate Cost (INR) Urine Routine + Culture ₹300–₹700 Consultation (Urologist/Gynecologist) ₹500–₹1500 Antibiotics (5-day course) ₹250–₹800 Ultrasound if needed ₹800–₹2000 UTIs are highly common in Indian women but are also highly preventable and treatable. Early detection, proper hygiene, hydration, and awareness go a long way. If symptoms persist, don’t delay medical care—especially during pregnancy or post-menopause. FAQs 1. Can drinking cranberry juice cure a UTI? Cranberry juice may help prevent UTIs but cannot cure an existing infection. Always consult a doctor for antibiotics. 2. Why do women get UTIs more than men? Women have a shorter urethra, making it easier for bacteria to reach the bladder. 3. How can I prevent UTIs during travel in India? Carry personal toilet seat covers, use clean restrooms, drink lots of water, and urinate frequently.
Painful Periods (Dysmenorrhea): Causes and Effective Treatments
Dysmenorrhea, commonly known as painful periods, affects a significant number of women in India, impacting daily activities and quality of life. Understanding its causes and exploring effective treatments can help manage this condition more effectively. Types of Dysmenorrhea Primary Dysmenorrhea: Painful menstruation without an underlying medical condition, often beginning in adolescence. Secondary Dysmenorrhea: Menstrual pain caused by reproductive system disorders such as endometriosis or fibroids. Causes The primary cause of dysmenorrhea is the production of prostaglandins, hormone-like substances that trigger uterine contractions. High levels can lead to intense contractions and pain. Secondary dysmenorrhea may result from conditions like: Endometriosis: Tissue similar to the uterine lining grows outside the uterus. Fibroids: Noncancerous growths in the uterus. Pelvic Inflammatory Disease (PID): Infection of the reproductive organs. Symptoms Cramping pain in the lower abdomen Pain radiating to the lower back and thighs Nausea and vomiting Diarrhea or loose stools Headaches and dizziness Diagnosis Diagnosis involves a medical history review and physical examination. For secondary dysmenorrhea, additional tests like ultrasound or laparoscopy may be necessary. Treatment Options Medications: NSAIDs: Nonsteroidal anti-inflammatory drugs like ibuprofen reduce prostaglandin production, alleviating pain. Hormonal Contraceptives: Birth control pills can regulate or eliminate periods, reducing or eliminating pain. Lifestyle Modifications: Regular Exercise: Physical activity releases endorphins, natural painkillers that can alleviate menstrual pain. Dietary Changes: Reducing caffeine and alcohol intake, and increasing consumption of omega-3 fatty acids, fruits, and vegetables may help. Alternative Therapies: Heat Therapy: Applying a heating pad to the lower abdomen can relax muscles and reduce cramping. Acupuncture and Yoga: These practices may help in reducing stress and alleviating pain. Surgical Options: In severe cases of secondary dysmenorrhea, surgical interventions like laparoscopy to remove endometrial tissue may be considered. When to See a Doctor Consult a healthcare provider if: Menstrual pain is severe and disrupts daily life Symptoms have worsened over time Over-the-counter medications are ineffective Dysmenorrhea is a prevalent issue among Indian women, but with the right knowledge and approach, it can be effectively managed. Combining traditional practices with modern medicine, maintaining a healthy lifestyle, and seeking timely medical advice are key to alleviating menstrual pain and improving quality of life. FAQs Is it normal to have painful periods? Mild discomfort is common, but severe pain that interferes with daily activities may indicate an underlying condition and should be evaluated. Can stress exacerbate menstrual pain? Absolutely. Stress can lead to hormonal imbalances, which may intensify menstrual cramps. Incorporating stress-reducing practices like yoga and meditation can be beneficial. Is it safe to exercise during menstruation? Yes, engaging in light to moderate exercise during menstruation can help reduce cramps and improve mood. Activities like walking, stretching, and yoga are particularly effective.
Irregular Periods: Causes, Symptoms, and When to See a Doctor
Menstrual cycles are a vital indicator of a woman’s reproductive health. While some variation is normal, consistently irregular periods can signal underlying health issues. This blog delves into the causes, symptoms, and guidance on when to seek medical attention. What Constitutes an Irregular Period? A typical menstrual cycle ranges from 21 to 35 days. Irregular periods may involve: Cycle Length Variability: Significant changes in cycle duration. Missed Periods: Skipping one or more cycles. Excessive Bleeding: Heavy flow requiring frequent pad changes. Spotting: Bleeding between periods. Common Causes Polycystic Ovary Syndrome (PCOS): Hormonal disorder causing enlarged ovaries with small cysts. Thyroid Disorders: Both hypothyroidism and hyperthyroidism can disrupt menstrual cycles. Stress and Lifestyle Factors: High stress, significant weight changes, and excessive exercise. Perimenopause: Transition phase before menopause. Medications: Certain drugs can affect hormone levels. Symptoms to Watch For Heavy Menstrual Bleeding: Soaking through pads or tampons every hour. Prolonged Periods: Lasting more than seven days. Severe Cramping: Intense pain during menstruation. Absence of Periods: No menstruation for three or more months. Diagnosis Evaluation may include: Medical History: Detailed menstrual and health history. Physical Examination: Including pelvic exam. Laboratory Tests: Hormone levels, thyroid function tests. Imaging: Ultrasound to assess reproductive organs. Treatment Options Lifestyle Modifications: Diet and Exercise: Maintaining a healthy weight. Stress Management: Techniques like yoga and meditation. Medications: Hormonal Therapies: Birth control pills to regulate cycles. Metformin: Especially in PCOS cases. Surgical Interventions: For Structural Issues: Such as fibroids or polyps. When to Consult a Doctor Seek medical advice if: Periods are absent for three or more months. Menstrual cycles are consistently irregular. Experiencing heavy bleeding or severe pain. FAQs Can irregular periods affect fertility? Yes, irregular ovulation can make it harder to conceive. Are irregular periods normal during adolescence? Some irregularity is common during puberty, but persistent issues should be evaluated. Can diet influence menstrual regularity? Yes, a balanced diet supports hormonal balance, which can regulate periods.
Pap Smear vs. HPV Test: What’s the Difference
Cervical cancer remains a leading cause of cancer-related deaths among women globally. Early detection through regular screenings can significantly reduce the risk. Two primary tests are employed for this purpose: the Pap Smear and the HPV Test. While both aim to prevent cervical cancer, they function differently. This article delves into their distinctions, procedures, and importance. What is a Pap Smear? A Pap Smear, or Pap test, involves collecting cells from the cervix to detect precancerous or cancerous changes. It’s a preventive measure to identify abnormal cells before they develop into cancer. The procedure is straightforward: A speculum is inserted into the vagina to visualize the cervix. A brush or spatula collects cervical cell samples. The sample is sent to a laboratory for analysis. Regular Pap Smears have been instrumental in reducing cervical cancer rates by facilitating early intervention. What is an HPV Test? The Human Papillomavirus (HPV) test detects the presence of high-risk HPV strains known to cause cervical cancer. Unlike the Pap Smear, which looks for cell changes, the HPV test identifies the virus responsible for these changes. The procedure is similar: Cell samples are collected from the cervix. The sample is tested specifically for high-risk HPV DNA. HPV infections are common, and most are cleared by the immune system. However, persistent infections with high-risk strains can lead to cervical cancer, making HPV testing crucial. Key Differences Between Pap Smear and HPV Test Aspect Pap Smear HPV Test Purpose Detects abnormal cervical cells Identifies high-risk HPV strains Method Cytological examination of cervical cells Molecular detection of HPV DNA Age Recommendation Begins at age 21 Often recommended for women 30 and older Frequency Every 3 years if results are normal Every 5 years if combined with Pap Smear (co-testing) Result Interpretation Identifies cell changes that may require further testing or monitoring Detects HPV presence; positive results may lead to additional screenings Why Are These Tests Important? Regular cervical screenings are vital because Early Detection: Identifying abnormal cells or HPV infections early allows for timely intervention, preventing progression to cancer. Preventive Care: Screenings can detect issues before symptoms arise, emphasizing prevention over treatment. Reduced Mortality Rates: Countries with regular screening programs have seen significant declines in cervical cancer cases and deaths. Current Guidelines and Recommendations In India, it’s recommended that: Women aged 21-29 undergo Pap Smear tests every three years. Women aged 30-65 consider co-testing (Pap Smear and HPV test) every five years or a Pap Smear alone every three years. Women over 65 with a history of normal results may discontinue screening It’s essential to consult with healthcare providers for personalized recommendations. FAQs Can I get an HPV test instead of a Pap Smear? While both tests serve different purposes, combining them (co-testing) provides comprehensive screening. However, consult your healthcare provider for personalized advice. Is the HPV vaccine a substitute for regular screenings? No, the HPV vaccine protects against certain strains of the virus but doesn’t eliminate the need for regular cervical screenings. Are these tests painful? Both procedures might cause mild discomfort but are generally not painful. Communicate any concerns with your healthcare provider.
When Should a Girl Have Her First Gynecologist Visit?
The transition into adolescence is a crucial time in a girl’s life — physically, emotionally, and hormonally. As puberty begins, new changes in the body require careful monitoring and understanding. One of the most common questions parents and guardians face is: When should a girl see a gynecologist for the first time? This is an important milestone, not just for reproductive health but for overall well-being. In this blog, we explore when and why girls should start seeing a gynecologist, what to expect during the first visit, and how early intervention can help prevent future health concerns. Why Early Gynecologist Visits Are Important Gynecological health is not just about reproduction. It includes menstruation, hormone regulation, breast health, and emotional well-being. An early visit helps in: Understanding normal vs abnormal menstruation Detecting early signs of infections or hormonal imbalances Educating teens about menstrual hygiene and reproductive health Providing guidance on safe sex and contraception if needed Building a trusted medical relationship for future concerns What Is the Right Age for the First Visit? According to the American College of Obstetricians and Gynecologists (ACOG), the first gynecologic visit should occur between the ages of 13 and 15 years, even if the girl is not sexually active. In India, many parents delay this visit unless there is a visible issue. However, preventive care is as important as treatment. Recommended Age: 13 to 15 years First period late or early? See a gynecologist if: No period by age 15 Period starts before age 9 Severe pain or irregular cycles Reasons for a First Gynecology Visit Here are some signs or situations that signal it’s time for the first visit: 1. Irregular or Painful Periods If a girl has: Periods that are very heavy or last longer than 7 days Extremely painful cramps Missed periods or no periods after age 15 These may indicate underlying issues like PCOS, thyroid dysfunction, or endometriosis. 2. Vaginal Discharge or Itching Unusual discharge, odor, or itching may be signs of a vaginal infection, often due to poor hygiene or hormonal changes. 3. Sexual Activity If a teenager becomes sexually active, a gynecologist can help with: Birth control counseling Sexually transmitted infection (STI) screening Safe sex education 4. Breast or Pelvic Pain Pain in the lower abdomen or breasts that affects daily activities can indicate hormonal problems or even cysts. 5. Concerns About Puberty Too early or delayed development (like breast growth or pubic hair) should be medically reviewed. What to Expect During the First Visit The first visit is often more of a conversation than a physical exam. The goal is to make the girl feel comfortable. It May Include: General health and menstrual history Discussion on hygiene, puberty, and changes Weight, height, and blood pressure checks External genital examination (if necessary) Pap smear or pelvic exam only if sexually active or symptomatic Reassure your child: “It’s okay to feel nervous. The doctor is here to help, not judge.” Parental Role in the Visit Parents should: Explain the reason for the visit in simple terms Allow privacy between the child and doctor if needed Avoid making the conversation taboo Respect the teenager’s privacy and let them build trust with the doctor independently. Top Tips for a Comfortable First Visit ✅ Choose a pediatric gynecologist or someone experienced with teens ✅ Talk to your daughter before the visit ✅ Prepare her for questions the doctor might ask ✅ Avoid showing fear or stigma around the topic Common Myths About First Gynecologist Visits Myth Reality Gynecologists are only for married women False – They help with puberty, periods, and more First visit means internal exam Not always. Usually, it’s a simple consultation It’s embarrassing A gynecologist is trained to make you comfortable Preventive Health Through Gynecology Routine check-ups help with: Detecting anemia from heavy periods Managing PCOS early Offering HPV vaccines Detecting cysts or reproductive tract abnormalities When to Follow Up The frequency of visits depends on health issues and symptoms. But generally: Annual visit for healthy girls More often if experiencing ongoing symptoms FAQs 1. Is it normal to feel nervous before the first gynecologist visit? Yes. It’s completely normal. A good gynecologist will talk first, help the teen feel at ease, and will not rush into physical exams unless absolutely necessary. 2. Should the mother accompany the child into the consultation room? Initially, yes. But the gynecologist may ask to speak privately with the teen to promote open conversation. It helps build trust. 3. What is the best time during the menstrual cycle to schedule the first visit? Ideally, avoid the period days unless there is an urgent issue. A few days after the period ends is often most comfortable.